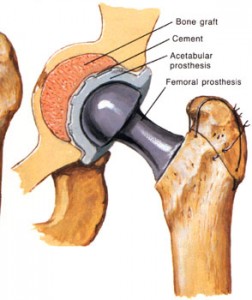
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant. Hip replacement surgery can be performed as a total replacement or a hemi replacement. Such joint replacement orthopaedic surgery generally is conducted to relieve arthritis pain or fix severe physical joint damage as part of hip fracture treatment. A total hip replacement (total hip arthroplasty) consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is currently the most successful and reliable orthopaedic operation with 97% of patients reporting improved outcome.
Total hip replacements are performed most commonly because of progressively worsening severe arthritis in the hip joint. The most common type of arthritis leading to total hip replacement is degenerative arthritis (osteoarthritis) of the hip joint. This type of arthritis is generally seen with aging, congenital abnormality of the hip joint, or prior trauma to the hip joint. Other conditions leading to total hip replacement include bony fractures of the hip joint, rheumatoid arthritis, and death (aseptic necrosis) of the hip bone. Hip bone necrosis can be caused by fracture of the hip, drugs (such as prednisone and prednisolone), alcoholism, and diseases (such as systemic lupus erythematosus).
The progressively intense chronic pain together with impairment of daily function including walking, climbing stairs, and even arising from a sitting position, eventually become reasons to consider a total hip replacement. Because replaced hip joints can fail with time, whether and when to perform total hip replacement are not easy decisions, especially in younger patients. Replacement is generally considered after pain becomes so severe that it impedes normal function despite use of anti-inflammatory and/or pain medications. A total hip joint replacement is an elective procedure, which means that it is an option selected among other alternatives. It is a decision which is made with an understanding of the potential risks and benefits. A thorough understanding of both the procedure and anticipated outcome is an important part of the decision-making process.
The risks of total hip replacement include blood clots in the lower extremities that can travel to the lungs (pulmonary embolism). Severe cases of pulmonary embolism are rare but can cause respiratory failure and shock. Other problems include difficulty with urination, local skin or joint infection, fracture of the bone during and after surgery, scarring and limitation of motion of the hip, and loosening of the prosthesis which eventually leads to prosthesis failure. Because total hip joint replacement requires anesthesia, the usual risks of anesthesia apply and include heart arrhythmias, liver toxicity, and pneumonia.
Total hip joint replacement can involve blood loss. Patients planning to undergo total hip replacement often will donate their own (autologous) blood to be banked for transfusion during the surgery. Should blood transfusion be required, the patient will have the advantage of having his or her own blood available, thus minimizing the risks related to blood transfusions. The preoperative evaluation generally includes a review of all medications being taken by the patient. Anti-inflammatory medications, including aspirin, are often discontinued one week prior to surgery because of the effect of these medications on platelet function and blood clotting. They may be reinstituted after surgery. Other preoperative evaluations include complete blood counts, electrolytes (potassium, sodium, chloride, bicarbonate), blood tests for kidney and liver functions, urinalysis, chest X-ray, EKG, and a physical examination. Your physician will determine which of these tests are required, based on your age and medical conditions. Any indications of infection, severe heart or lung disease, or active metabolic disturbances such as uncontrolled diabetes may postpone or defer total hip joint surgery.
Rehabilitation and physical therapy are started immediately following surgery and continue throughout hospitalization and at home for one year after surgery. On the first day after surgery, the physical therapist will meet with you in your hospital room for an assessment. On the second day, you will go to the Physical Therapy department by wheelchair for treatment. Your physical therapist will monitor the strength and flexibility in your leg and hip, as well as your ability to stand and sit. In addition, a physical therapist will provide goals and instructions for you to complete while in the hospital and at home.
Your doctor may determine that it is best for your recovery if you go to a rehabilitation center after discharge from the hospital. At the rehabilitation center, you will have concentrated time with a physical therapist and occupational therapist and will regain your strength, learn about all your exercises and the precautions that you’ll need to follow. Your length of stay at this facility is approximately five to 14 days. Your doctor’s physician assistant or nurse will discuss facilities available for your needs.
After total hip joint replacement surgery, patients often start physical therapy immediately! On the first day after surgery, it is common to begin some minor physical therapy while sitting in a chair. Eventually, rehabilitation incorporates stepping, walking, and climbing. Initially, supportive devices such as a walker or crutches are used. Pain is monitored while exercise takes place. Some degree of discomfort is normal. It is often very gratifying for the patient to notice, even early on, substantial relief from the preoperative pain for which the total hip replacement was performed.
Physical therapy is extremely important in the overall outcome of any joint replacement surgery. The goals of physical therapy are to prevent contractures, improve patient education, and strengthen muscles around the hip joint through controlled exercises. Contractures result from scarring of the tissues around the joint. Contractures do not permit full range of motion and therefore impede mobility of the replaced joint. Patients are instructed not to strain the hip joint with heavy lifting or other unusual activities at home. Specific techniques of body posturing, sitting, and using an elevated toilet seat can be extremely helpful. Patients are instructed not to cross the operated lower extremity across the midline of the body (not crossing the leg over the other leg) because of the risk of dislocating the replaced joint. They are discouraged from bending at the waist and are instructed to use a pillow between the legs when lying on the nonoperated side in order to prevent the operated lower extremity from crossing over the midline. Patients are given home exercise programs to strengthen the muscles around the buttock and thigh. Most patients attend outpatient physical therapy for a period of time while incorporating home exercises regularly into their daily living.
Occupational therapists are also part of the rehabilitation process. These therapists review precautions with the patients related to everyday activities. They also educate the patients about the adaptive equipment that is available and the proper ways to do their “ADLs” or activities of daily living.
© 2021 Singapore Orthopaedic Centre for Spine & Sports Medicine. All Rights Reserved.
Designed By ArsEmporium.com
Connect with Us